Taking Calcium Supplements Can Cause Brain Lesions
Taking Calcium Supplements Can Cause Brain Lesions
Taking calcium supplements — even at low doses — linked to brain lesions in the first study of its kind.
For the last several years, there has been ongoing controversy as to whether calcium supplementation is beneficial or harmful: probably the two areas where this gets the most focus would be related to osteopaenia/osteoporosis as well as the cardiovascular system.
The public has become increasingly confused on this topic, and such industries as the milk industry have spent considerable amounts of money to convince the general public of the benefits of consuming their products.
Unfortunately, the general public do not have the knowledge to understand that like many issues related to health trying to isolate a single factor like calcium consumption in relation to bone health does not take into consideration the complexity of our biochemistry and metabolism.
Bone health cannot be addressed without taking into consideration the fat soluble vitamins – but also a range of other co-factors.
To add further to the controversy surrounding the topic of isolated calcium supplementation, a recently published study suggests that this practice can in fact lead to the development of brain lesions.
The following article which profiles the fact that taking calcium supplements can cause brain lesions was published on the Green Med Info website:
Most calcium supplements are just plain bad news. The idea of taking calcium in pill or tablet form to “keep the bones strong” just doesn’t make that much sense given, first, that we are designed to get our calcium from food. Second, our bone is a living tissue, which requires vitamin C, amino acids, magnesium, silica, vitamins D and K, etc., not to mention regular physical activity, just as much as it does calcium. Taking calcium to the exclusion of these other critical factors doesn’t make sense; nor does it make sense to look at osteoporosis as a deficiency of calcium supplements!
As we have reported on extensively in the past, not only is consuming limestone, bone, and the shells of oysters and eggs not a good idea because the calcium can deposit in our soft tissues leading to heart attacks and strokes,
but even the goal of maintaining bones as dense as a 25-year old late into life (known as the T-score) is fraught with danger, including a far higher breast cancer risk for those with the highest bone density.
Instead of pathologizing aging, and focusing on making the bone denser by any means necessary, the focus should be on bone quality and agility and bodily self-awareness late into life, which helps the elderly prevent the falls that lead to fracture in the first place. In other words, simply having a gait or vision disorder can be at least as an important factor in fracture risk as bone mineral density.
The challenge with poor quality, inorganic, calcium supplements, however, does not stop with their contribution to cardiovascular disease risk. A combination of factors including low magnesium, vitamin K2 and the presence of fluoride in the water and diet can lead to pineal gland calcification, as well as the calcification of other brain structures, which recently has been hypothesized to be a contributing factor in the pathogenesis of Alzheimer’s disease.
Br J Nutr. 2014 Jul 28;112(2):220-7. doi: 10.1017/S0007114514000828. Epub 2014 Apr 30.
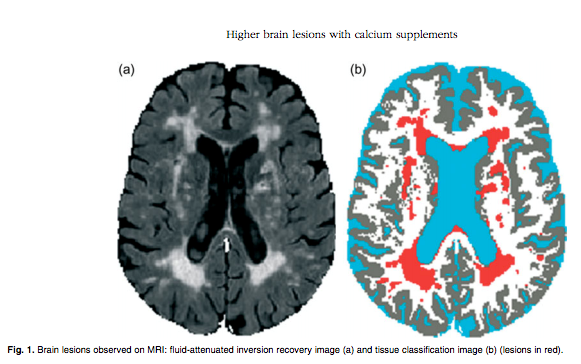
A truly provocative study on this topic published last year in the British Journal of Nutrition somehow slipped through the cracks, because not only did we miss it but we do not recall it being reported elsewhere. Titled, “Elevated brain lesion volumes in older adults who use calcium supplements: a cross-sectional clinical observational study,” the study looked at the possibility that since calcium supplements have now been linked in multiple studies with vascular pathologies associated with cardiovascular disease they may also be associated with the occurrence of brain lesions (known on MRI scans as hyperintensities) in older adults. These brain lesions, visible as brighter spots in MRI scans, are known to be caused by lack of blood flow (ischemia) and subsequent neurological damage.
According to the study,
“Brain lesions, also known as hyperintensities, are areas of damage observed on brain MRI (See Above). These lesions are common in older adults and increase the risk of devastating health outcomes, including depression, cognitive decline, dementia, stroke, physical disability, hip fracture and death. Postmortem studies have determined that these lesions form primarily due to ischemia, especially larger lesions (.3mm) and lesions found in depressed individuals.”
The observational study enrolled 227 older adults (60 years above) and assessed food and supplemental calcium intakes. Participants with supplemental calcium use above zero were categorized as supplement users. Lesion volumes were assessed with MRI scans.
Key findings were:
- Greater lesion volumes were found among calcium supplement users than non-users
- The influence of calcium supplements was of a magnitude similar to that of the influence of high blood pressure (hypertension), “a well-established risk factor for lesions.”
- The study found that the amount of calcium used was not associated with lesion volume and that “even low-dose supplements, by older adults may be associated with greater lesion volumes.”
- Even after controlling for food calcium intake, age, sex, race, years of education, energy intake, depression and hypertension, the association between calcium supplement and lesion volumes held strong.
Here is the abstract of this study:
Br J Nutr. 2014 Jul 28;112(2):220-7. doi: 10.1017/S0007114514000828. Epub 2014 Apr 30.
Payne ME1, McQuoid DR1, Steffens DC2, Anderson JJ3.
Abstract
Recent studies have implicated Ca supplements in vascular risk elevation, and therefore these supplements may also be associated with the occurrence of brain lesions (or hyperintensities) in older adults. These lesions represent damage to brain tissue that is caused by ischaemia. In the present cross-sectional clinical observational study, the association between Ca-containing dietary supplement use and lesion volumes was investigated in a sample of 227 older adults (60 years and above). Food and supplemental Ca intakes were assessed with the Block 1998 FFQ; participants with supplemental Ca intake above zero were categorised as supplement users. Lesion volumes were determined from cranial MRI (1.5 tesla) scans using a semi-automated technique; volumes were log-transformed because they were non-normal. ANCOVA models revealed that supplement users had greater lesion volumes than non-users, even after controlling for food Ca intake, age, sex, race, years of education, energy intake, depression and hypertension (Ca supplement use: β = 0.34, SE 0.10, F(1,217)= 10.98, P= 0.0011). The influence of supplemental Ca use on lesion volume was of a magnitude similar to that of the influence of hypertension, a well-established risk factor for lesions. Among the supplement users, the amount of supplemental Ca was not associated with lesion volume (β = – 0.000035, SE 0.00 015, F(1,139)= 0.06, P= 0.81). The present study demonstrates that the use of Ca-containing dietary supplements, even low-dose supplements, by older adults may be associated with greater lesion volumes. Evaluation of randomized controlled trials is warranted to determine whether this relationship is a causal one.
PMID: 24787048 PMCID: PMC4144340
This study reinforces for all of us the importance of patient education: as we all know, patients often engage in what they believe will be health enhancing activities whereas in reality just the opposite may be true.
We won’t address in any great depth in this article the biochemistry/physiology of bone health (it is readily available from many sources, including the link below to an article from the Linus Pauling Institute), however we will address some of the associated co-factors besides calcium which are important for bone health.
The following paper provides a good overview of the importance of Vitamins D and K to bone health.
Fat soluble vitamins for maintaining bone health
Abstract
Vitamin D and K are nutrients necessary for bone health. Vitamin D insufficiency, which is milder than vitamin D deficiency to cause rickets and osteomalacia, is associated with increased fracture risk. Serum 25 (OH) D concentration, a good marker for vitamin D status, must be higher than the traditional held consensus of 20 ng/mL for bone health. Daily dose of 800 IU or higher is considered to be necessary for fracture prevention. Recently, much attention has been paid on extra-hepatic actions of vitamin K including bone. Elevated serum concentration of undercarboxylated osteocalcin, a sensitive marker for vitamin K inadequacy in the bone, is a risk factor for fracture independent of bone mineral density.
The following article, written by Chris Masterjohn, PhD provides some good imformation related to the significance of additional co-factors involved in bone health (such as Vitamin C, magnesium, zinc, fat and carbohydrate, as well as important metabolic factors such as carbon dioxide and thyroid hormone)
If you are not familiar with Chris, he is definitely worth making note of:
He holds a PhD in Nutritional Science and is very involved with the Weston A. Price Foundation so he approaches health and nutrition from an ancestral health/whole food paradigm.
He has written some very insightful articles on the fat soluble vitamins, and his blog, The Daily Lipid and his website Cholesterol and Health (link below) always provide great information and articles.
Nutritional Adjuncts to the Fat-Soluble Vitamins A, D, and K
About the Author
Chris Masterjohn has a PhD in nutritional sciences from the University of Connecticut, and has published five peer-reviewed papers on vitamins and supplementation. He researches fat-soluble supplements – A, D, and K – at the University of Illinois. He also maintains a blog, The Daily Lipid, and his website, Cholesterol-And-Health.com, which are dedicated to the issue of cholesterol. He’s also active with the Weston A. Price Foundation.
Another great resource for matters relating to health and nutrition from a research perspective is the reference material available through the Linus Pauling Institute at the University of Oregon from which the following article on micronutrients and bone health comes from.
Micronutrients and Bone Health – Linus Pauling Institute, University of Oregon
There is no doubt that bone health is a significant health issue, especially with the aging population as bone loss/osteopenia/osteoporosis is a significant problem:
Here are some statistics from the International Osteoporosis Society website:
Due to its prevalence worldwide, osteoporosis is considered a serious public health concern. Currently it is estimated that over 200 million people worldwide suffer from this disease1. Approximately 30% of all postmenopausal women have osteoporosis in the United States and in Europe. At least 40% of these women2 and 15-30% of men3 will sustain one or more fragility fractures in their remaining lifetime. Ageing of populations worldwide will be responsible for a major increase in the incidence of osteoporosis in postmenopausal women4.
It has been shown that an initial fracture is a major risk factor for a new fracture. An increased risk of 86% for any fracture has been demonstrated in people that have already sustained a fracture5. Likewise, patients with a history of vertebral fracture have a 2.3-fold increased risk of future hip fracture and a 1.4-fold increase in risk of distal forearm fracture6.
This position statement from the American Academy of Orthopaedic Surgeons provides an interesting perspective on this topic (although probably most of us would take a more natural approach to this issue via diet, exercise and supplementation vs. the prescription drug approach with some of the bisphosphonates and other related compounds which can cause serious side effects and there has been recent controversy as to whether they are beneficial at reducing fracture rates.
Position Statement
Osteoporosis/Bone Health in Adults as a National Public Health Prioritoy
American Academy of Orthopaedic Surgeons
Based upon current scientific knowledge about osteoporosis, it is further believed physician education programs should include the following information:
Risk factors associated with osteoporosis including
- Insufficient calcium intake
- Vitamin D deficiency
- Sedentary lifestyle
- Smoking
- Excessive alcohol consumption
- Family history of fractures
- Loss of endogenous sex hormones
- Chronic glucocorticoid use
- A small, slender body
- Caucasian, Hispanic, Native American, or Asian American ethnicity
- All ethnic groups need to be considered at risk for metabolic bone disease, including but not limited to osteoporosis
- The importance of adequate dietary intake of calcium, vitamin D and other nutrients, starting at an early age, especially for young girls
- Testing of blood levels of these nutrients should be considered even in the young and in all ethnic groups, especially if there is significant fracture history
- Emphasis on diagnosis of other, possibly co-existing metabolic bone diseases
- Efficacy and safety of current estrogen and other hormone and estrogen receptor modifiers (SERMs) to prevent and treat osteoporosis
- Efficacy and safety of bisphosphonates, calcitonin, biologics, teriparatide, and evolving therapies to prevent and treat osteoporosis
- Guidelines on sufficient exercise and activity
- Fall prevention strategies and rehabilitation, including safety education, vision, and hearing checks
Clinicians need to be cognizant that all ethnic groups are susceptible to osteoporosis, and the disease is under diagnosed in the African American population. Based on nationally representative estimates, a considerable proportion of people with osteoporotic fractures have not received a diagnosis of osteoporosis (prior to or after their fracture). This is especially true among males and African Americans. Early diagnosis of osteoporosis is usually established by a combination of a complete medical history and physical examination, skeletal radiographs, bone densitometry and specialized laboratory tests.
The care for patients with established osteoporosis should include:
- Early diagnosis of potentially treatable secondary types of osteoporosis
- Decreasing fracture risk by utilizing medications, such as SERMs, bisphosphonates, denosumab, teriparatide
- Exercise and activity programs
- Injury prevention strategies
- Optimizing nutrition and lifestyle variables to decrease risk
While there is much to be learned about the causes of osteoporosis, there is sufficient current knowledge to undertake therapeutic action today. Effective new regimens that stimulate bone formation will require increased federal research support. Recent studies have shown the declining rates of osteoporosis management following fragility fractures from 2000-2009 in the US. While primary fracture prevention is the goal, secondary prevention is critical to prevent the future costs to the patient and society. Every orthopaedic surgeon should work diligently to participate in prevention and treatment of osteoporosis and fragility fracture care.
Biotics Research offers a number of formulations targeted at bone health, which include:
Ca/Mg Plus
Regards,
Rob Lamberton

Robert Lamberton Consulting
Functional Medicine Consultant: Biotics Research
Product Formulator of Professional Nutraceutical Products
Certified Light/Darkfield Microscopy Nutritionist
Author of the Biotics Canada Newsletter Articles
Contributing Writer / Advisory Board Member:
Nutricula: The Science of Longevity Journal
Healthy Organic Woman Magazine
Twitter: rob_lamberton Skype: larch60
Email: Rob@BioticsCan.com
Phone: 778-227-4952
References
- Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992 Nov;2(6):285-9
2. Melton III LJ, Chrischilles EA, Cooper C, Lane AW, Riggs BL: Perspective: How many women have osteoporosis? J Bone Miner Res 1992;7:1005-10
3. Randell A, Sambrook PN, Nguyen TV, Lapsey H, Jones G, Kelly PJ, Eisman JA. Direct clinical and welfare costs of osteoporotic fractures in elderly men and women. Osteoporosis Int 1995;5:427-32
4. Reginster JY. Burlet N. Osteoporosis: A still increasing prevalence. Bone 2006;38: S4-S9
5. Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas PD, Eisman JA, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A. A meta-analysis of previous fracture and subsequent fracture risk. Bone 2004;35(2):375-82
6. Melton III LJ, Atkinson EJ, Cooper C, O’Fallon WM, Riggs BL. Vertebral fractures predict subsequent fractures. Osteoporosis Int 1999;10:214-21
Tags: Brain Health