Overview
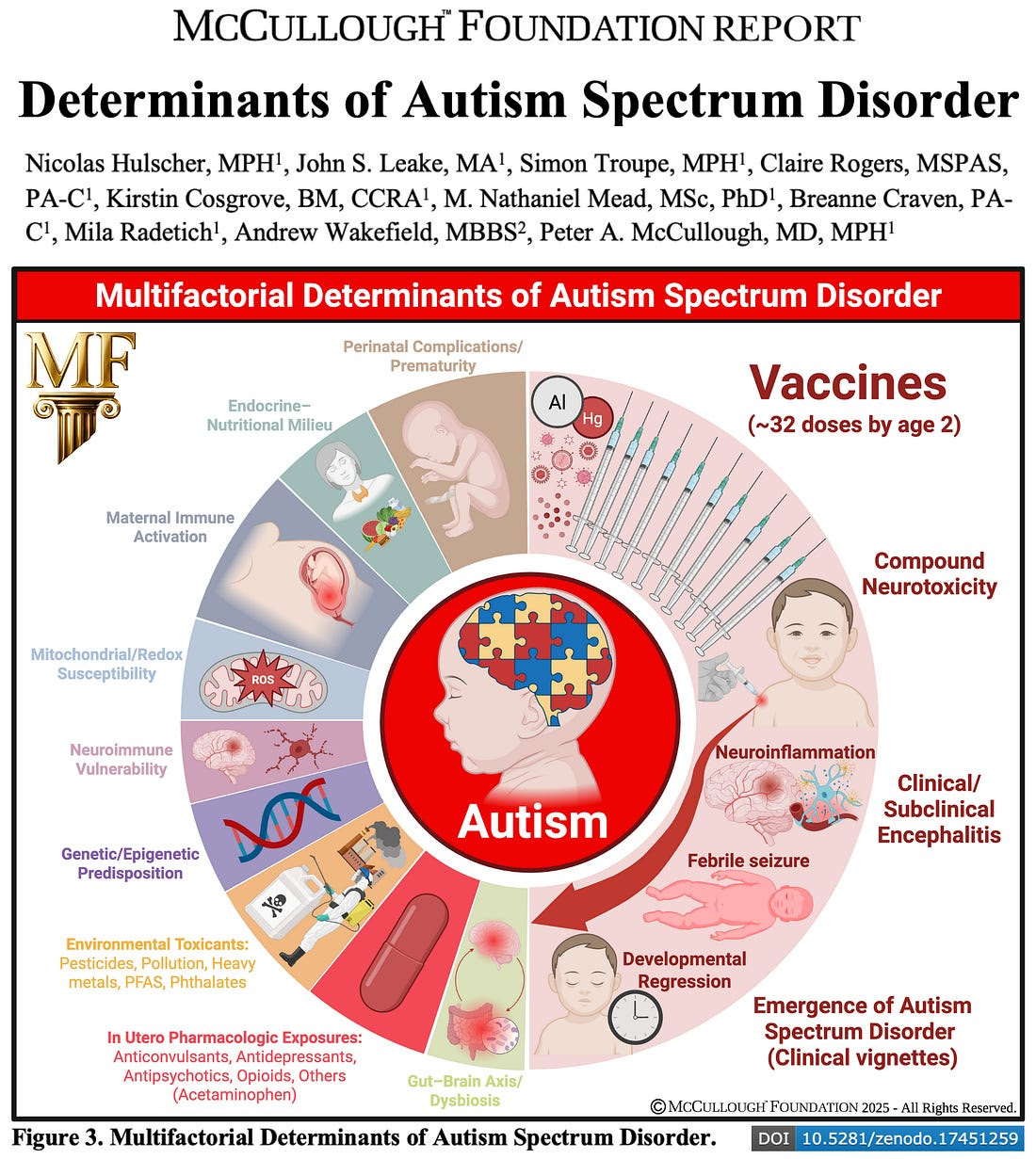
The McCullough Foundation’s latest meta-analysis, led by Nicolas Hulscher, MPH, and a multidisciplinary research team, reviews over 300 studies examining possible causes of autism. This comprehensive synthesis maps genetic, environmental, immune, and vaccine-related risk factors, offering an unprecedented perspective on Autism Spectrum Disorder (ASD).
Key Findings
- Vaccine Studies:
Out of 136 scientific studies on vaccines, 107 (79%) found evidence for a possible vaccine-ASD link. - Unvaccinated vs. Vaccinated Children:
Twelve studies directly compared fully vaccinated with completely unvaccinated children; all reported significantly better overall health—including lower ASD risks—in the unvaccinated group. - Mechanistic Evidence:
Studies reveal converging mechanisms such as immune dysregulation, mitochondrial stress, and neuroinflammation triggered by vaccine components during critical periods of brain development. - Other ASD Risk Factors:
Older parental age, prematurity, genetics, toxins, maternal immune activation, drug exposure, and gut-brain axis changes play confirmed but less dominant roles. None fully explain the surge in autism prevalence coinciding with the expansion of pediatric vaccine schedules in the U.S. after 1986. - Research Gaps:
No study has yet reviewed the full cumulative pediatric vaccine schedule for long-term neurodevelopmental outcomes.
Practitioner Insight
As both public demand and clinical questions about ASD continue to grow, practitioners are uniquely positioned to guide nuanced, evidence-informed discussions with families. This report highlights the need for:
- Thorough evaluation and communication about all potential ASD risk factors—including vaccine-related exposures—while respecting individual family circumstances.
- Advocacy for comprehensive, unbiased research, especially studies with truly unvaccinated control groups and full-schedule assessments.
- Monitoring of neurodevelopmental health in patients—especially those with family risk factors or early-life exposures—using both conventional and integrative approaches to prevention and wellness.
Healthcare professionals are encouraged to stay updated on emerging research, support informed shared decision-making, and maintain vigilance for new data guiding practice and policy.
Call to Action
For Practitioners:
- Review the full McCullough Foundation report and related press releases (see References below).
- Consider discussing these findings with peers and in professional forums to foster critical dialogue and ethical research priorities.
- Urge research institutions and policymakers to prioritize long-term studies addressing the cumulative impact of the pediatric vaccine schedule.
For Families and the Public:
- Seek out reputable sources and read the full report to understand the multifactorial nature of ASD risk.
- Discuss all health and vaccine decisions—and concerns—openly with trusted healthcare providers.
- Join advocacy efforts calling for comprehensive autism and vaccine safety research.
Together, the healthcare community and the public can support a new era of transparency and scientific rigor for the benefit of children’s health.
References & Further Reading
- Full McCullough Foundation report: Zenodo Repository
Author Acknowledgments:
Nicolas Hulscher, MPH, John S. Leake, MA, Simon Troupe, MPH, Claire Rogers, MSPAS, PA-C, Kirstin Cosgrove, BM, CCRA, M. Nathaniel Mead, MSc, PhD, Bre Craven, PA-C, Mila Radetich, Andrew Wakefield, MBBS, and Peter A. McCullough, MD, MPH, with thanks to the Bia-Echo Foundation.