Dietary intervention restores protective protein and decreases death rate in mice
Source: Society for Neuroscience
The incidence of dementia and Alzheimer’s continues to escalate in the general population.
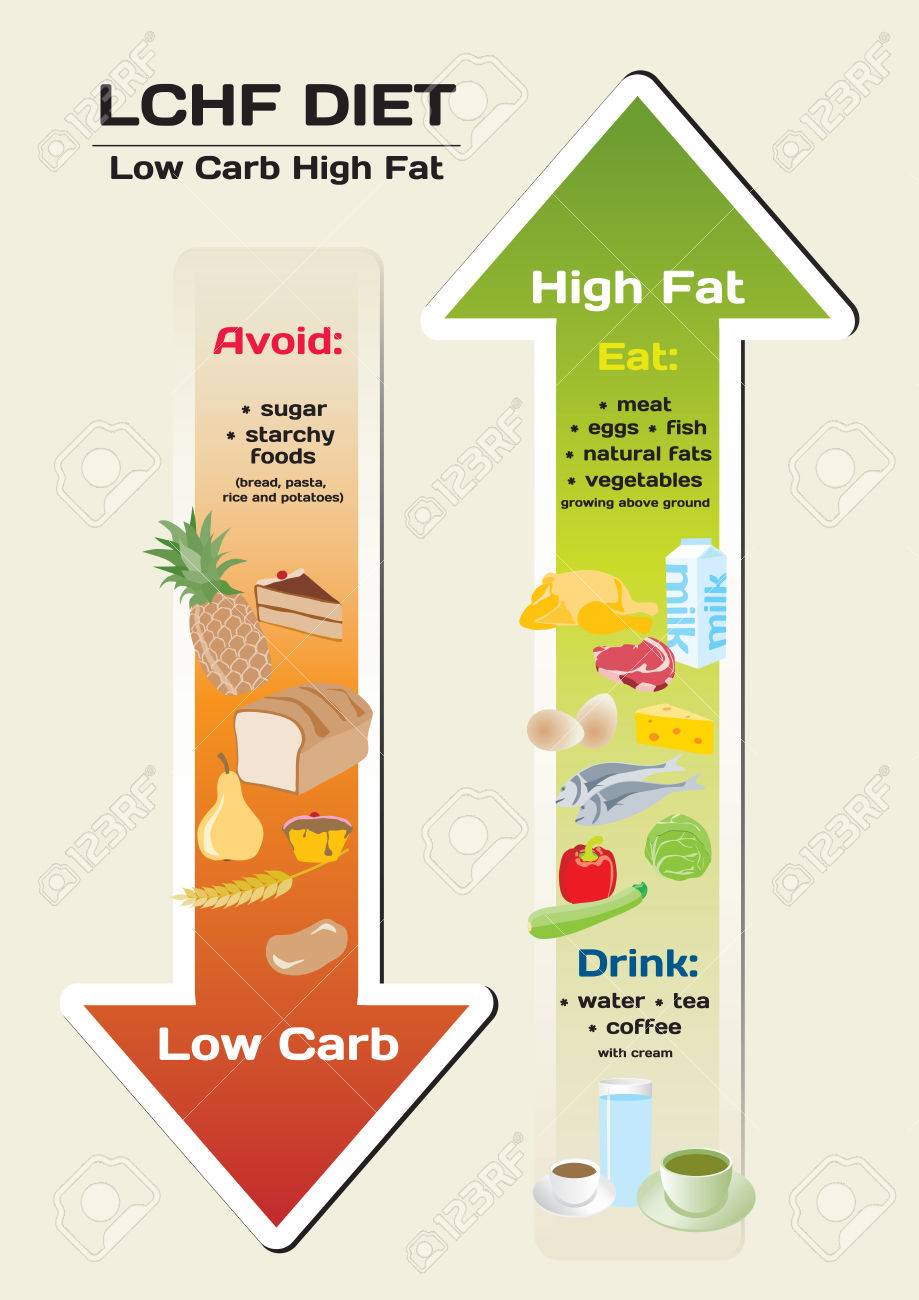
LCHF/Keto diets have proven to be beneficial to individuals dealing with these health issues.
It has been suggested that these conditions may partly be due to impaired glucose metabolism in the brain, hence the increasing use of the term “Type 3 Diabetes”.
Enabling the brain to use ketones for its energy source therefore can provide some benefit with regards to brain function.
A major challenge with this is that a radical dietary shift in the geriatric population can be quite challenging – if not impossible.
Usage of exogenous ketone compounds is one potential option in this situation.
Following is an article from Science Daily which talks about published research which suggests that increasing ketone levels in the diet can help to protect neurons from death during the progression of Alzheimer’s disease.
Summary: A ketone-supplemented diet may protect neurons from death during the progression of Alzheimer’s disease, according to research in mice.
A ketone-supplemented diet may protect neurons from death during the progression of Alzheimer’s disease, according to research in mice recently published in JNeurosci.
Early in the development of Alzheimer’s disease, the brain becomes over excited, potentially through the loss of inhibitory, or GABAergic, interneurons that keep other neurons from signaling too much. Because interneurons require more energy compared to other neurons, they may be more susceptible to dying when they encounter the Alzheimer’s disease protein amyloid beta. Amyloid beta has been shown to damage mitochondria — the metabolic engine for cells — by interfering with SIRT3, a protein that preserves mitochondrial functions and protects neurons.
Cheng et al. genetically reduced levels of SIRT3 in mouse models of Alzheimer’s disease. Mice with low levels of SIRT3 experienced a much higher mortality rate, more violent seizures, and increased interneuron death compared to the mice from the standard Alzheimer’s disease model and control mice. However, the mice with reduced levels of SIRT3 experienced fewer seizures and were less likely to die when they ate a diet rich in ketones, a specific type of fatty acid. The diet also increased levels of SIRT3 in the mice.
Increasing SIRT3 levels via ketone consumption may be a way to protect interneurons and delay the progression of Alzheimer’s disease.
Story Source:
Materials provided by Society for Neuroscience. Note: Content may be edited for style and length.
Journal Reference:
- Aiwu Cheng, Jing Wang, Nathaniel Ghena, Qijin Zhao, Isabella Perone, M. Todd King, Richard L. Veech, Myriam Gorospe, Ruiqian Wan, Mark P. Mattson. SIRT3 Haploinsufficiency Aggravates Loss of GABAergic Interneurons and Neuronal Network Hyperexcitability in an Alzheimer’s Disease Model. The Journal of Neuroscience, 2019; 1446-19 DOI: 10.1523/JNEUROSCI.1446-19.2019
Abstract
SIRT3 Haploinsufficiency Aggravates Loss of GABAergic Interneurons and Neuronal Network Hyperexcitability in an Alzheimer’s Disease Model
Impaired mitochondrial function and
aberrant neuronal network activity are believed to be early events in
the pathogenesis of Alzheimer’s disease (AD), but how mitochondrial
alterations contribute to aberrant activity in neuronal circuits is
unknown. In this study, we examined the function of mitochondrial
protein deacetylase sirtuin 3 (SIRT3) in the pathogenesis of AD.
Compared to AppPs1 mice, Sirt3-haploinsufficient AppPs1 mice
(Sirt3+/-AppPs1) exhibit early epileptiform EEG activity and Seizure.
Both male and female Sirt3+/-AppPs1 mice were observed to die
prematurely before five months of age.
When comparing male mice among different genotypes, Sirt3
haploinsufficiency renders GABAergic interneurons in the cerebral cortex
vulnerable to degeneration and associated neuronal network
hyperexcitability. Feeding Sirt3+/-AppPs1 AD mice with a ketone
ester-rich diet increases SIRT3 expression and prevents seizure-related
death and the degeneration of GABAergic neurons, indicating that the
aggravated GABAergic neuron loss and neuronal network hyperexcitability
in Sirt3+/-AppPs1 mice are caused by SIRT3 reduction and can be rescued
by increase of SIRT3 expression. Consistent with a protective role in
AD, SIRT3 levels are reduced in association with cerebral cortical Aβ
pathology in AD patients. In summary, SIRT3 preserves GABAergic
interneurons and protects cerebral circuits against hyperexcitability,
and this neuroprotective mechanism can be bolstered by dietary ketone
esters.
SIGNIFICANCE STATEMENT
GABAergic neurons provide the main
inhibitory control of neuronal activity in the brain. By preserving
mitochondrial function, SIRT3 protects parvalbumin and calretinin
interneurons against Aβ-associated dysfunction and degeneration in
AppPs1 AD mice, thus restraining neuronal network hyperactivity. The
neuronal network dysfunction that occurs in AD can be partially reversed
by physiological, dietary, and pharmacological interventions to
increase SIRT3 expression and enhance the functionality of GABAergic
interneurons.